The Gut Microbiome: The Trillions of Microbes that Tell Your Body What to Do
Microbes in our guts control immunity, help us access vitamins and amino acids, protect us from toxins and inflammation, and communicate with our brains
Functionally speaking, your gut is your root system. For humans, both the gut microbiome and the soil microbiome are vitally important to growth, immunity, and metabolism. For both plants and humans, their microbial relationships bring nutrients and compounds to their host that they wouldn’t be able to access otherwise. They also convert nutrients and compounds into forms the person or plant’s body can use.
Healthy top soils contain about 100 billion microbes per teaspoon of soil! These microbes are absolutely essential to cycling death back into life, keeping the raw materials needed for life in constant circulation. Unfortunately, industrial agriculture leads to similar impacts on both soil microbiomes and human microbiomes. We transitioned away from fiber-rich nourishment for soil microbes like mulch, compost, and manure. Then, we replaced it with processed versions of nutrients like chemical fertilizers. This has had a dramatic effect on soil health and microbes.
In addition, herbicides like glyphosate (Round-Up) were considered not to impact human health because the pathway it acts on in plants is not present in humans. However, 54% of microbes considered “core” to the human microbiome are impacted by glyphosate and the chemicals it breaks down into. Animal studies showed that animals fed high doses of glyphosate led to a significant decrease in Lactobacillus species of bacteria. Anxiety and depressive behaviors followed for mice after the decrease. Some people think that the large increase in gluten intolerance is not due to the gluten in wheat, but the large amounts of Round-Up sprayed on wheat shortly before harvest.
Similarly, we have replaced fiber-rich foods like green, leafy vegetables and whole grains, with their processed equivalents, sometimes with chemical nutrients added (like multivitamins or fortified cereals and flours). People ate the same amount of carbohydrates in 1997 as they did in 1909. However, the nature of these carbohydrates was dramatically different as food manufacturers removed fiber and phytochemicals from food in favor of sugars and simple starches. In fact, in the United States 60% of our calories come from ultra-processed foods. This has had a major impact on the health of human microbiomes, human bodies, and human communities.
When microbiomes are thriving, the healthy bacteria significantly outnumber disease causing bacteria. They prevent proliferation of disease-causing bacteria through:
Physical displacement
Resource deprivation
Chemical deterrence
Activation of host immunity
However, like in human communities, it’s complicated. Many microbes are not all good or all bad. For example, species in the genus Parabacteroides protects against cancer, decreases the likelihood of obesity, but can help or harm in Crohn’s, ulcerative colitis, diabetes, heart disease, and autoimmune diseases.
When plants have less effective defense responses and soil can’t cycle nutrients properly. Likewise, when harmful bacteria take over a human gut, people develop abnormal immune and metabolic responses. Communication between immune cells in the gut and the microbes in the gut is critical to how the immune system functions. When the communication is going well, the immune system provides a balanced response, acting upon real threats, without over-responding to human tissues or allergens. If the response is too vigorous autoimmune illnesses develop. If it is too weak, there is increased risk of infection or cancer.
Fiber is the key to a healthy microbiome, but it’s not just the fiber in your diet, but also in that of your recent ancestors that may impact your microbiome. In studies of mice colonized with human gut microbes, they fed four generations of mice progressively smaller amounts of fiber in their diet. Some of the fiber-dependent groups of microbes were entirely gone by the last generation. They did not return simply by adding fiber back into the diet, but would return if the bacteria was re-introduced at the same time that fiber was increased.
The human gut is host to 2766 different species of bacteria, numbering, in total, 10 to 100 trillion organisms. Each person has a unique microbial community that is first populated when passing through the birth canal and through breast milk. A person’s DNA can influence which microbes survive and thrive there. However, only 8% of the gut composition is suspected to be related to inherited genes.
The microbes in our guts are tremendously important. They have so many important jobs and control so many important systems that they make the line between “me” and “not me” very blurry. Here are a few of the important tasks of the gut microbiome:
Stimulate the immune system
Breakdown potentially toxic food compounds
Create or convert other compounds into important neurotransmitters (chemicals that communicate in the nervous system)
Make vitamins and amino acids
Enzymes needed to form vitamin B12 are only found in bacteria, not plants or animals. One research team found that 86% of vitamin B6, 37% of vitamin B9, 31% of vitamin B12, and 27% of vitamin B3 are provided by but microbes. Overall, ⅓ to nearly 40% of all human metabolites (the products made as a result of converting food and drink into energy) are produced by the gut microbiome. In addition, these metabolites are critical to the function of immune, endocrine (hormonal), and nervous system cells.
Digestion and the Critical Role of Short-Chain Fatty Acids
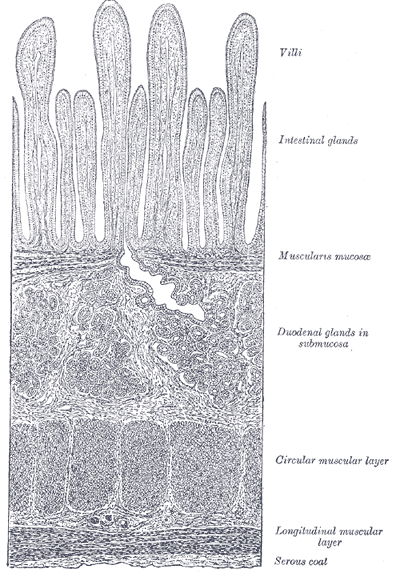
The top portion of your small intestine absorbs the sugars (like table sugar, sugar from fruits or milk). Some starches and fibers are more difficult to digest. These often pass into the large intestine (colon), where microbes use enzymes to help break down the materials. The fibers that can’t be digested undergo fermentation. This leads to the production of short-chain fatty acids.
Short-chain fatty acids are a group of chemicals including lactate, butyrate, acetate, and propionate. They are mostly produced by bacteria in the colon. They are involved in communication about energy expenditure in the muscles and liver. High levels of short-chain fatty acids are associated with decreased anxiety and depression symptoms and low levels are associated with an increase in anxiety and depression symptoms. They prevent infection with a type of bacteria called Shigella, which can cause severe diarrheal illness. Butyrate has several important jobs for the function of the intestines including:
Keeping the barrier made by the intestines strong
Maintaining the right level of oxygen to maintain healthy intestinal microbe communities
Decreases inflammation
Maintains the integrity of the blood brain barrier
Triggers the release hormones that maintain blood sugar levels, signals the feeling of satiety, and manages fat storage
Diets that support bacteria that produce short-chain fatty acids have been shown to improve conditions like high blood pressure, asthma, non-alcoholic fatty liver disease, and several mental health conditions.
Butyrate and Inflammation
The wall of the intestines is only one cell-layer thick. When the colon is not producing enough butyrate, it is difficult for the colon cells to stay close enough together to form an effective barrier. It is also difficult for those cells to create the mucus needed as an additional layer of protection. When these protective barriers aren’t in place, material from inside the intestines can get to the brain, lungs, liver, and many other sites in the body. This provokes an inflammatory response. In other words, nourishing these colon bacteria can reduce inflammation throughout the body. This low-level inflammation plays a role in many chronic diseases including:
Type 2 diabetes
Heart disease
Asthma
Eczema
Depression
Irritable bowel syndrome
Some neurologic diseases (like Alzheimer’s and Parkinson’s)
Obesity (In other words, people who tell you weight= calories in- calories out are missing a key part of the equation)
Some cancers
Chronic Pain and the Microbiome
Recent animal research suggests that the microbes in the gut have play a role in the development of pain originating from the internal organs, nerve pain due to chemotherapy, and the dose of opioids that will effectively relieve pain (opioid tolerance). Human studies have found changes in the microbiome in patients with irritable bowel syndrome, chronic pelvic pain, rheumatoid arthritis, and chronic fatigue syndrome.
Fibromyalgia is a chronic pain condition that involves pain and tenderness throughout the body, fatigue, sleep disturbances, and brain fog. For years, people with fibromyalgia have dealt with a medical system that often disbelieves their experience or is frankly antagonistic to their experience and their needs. Recently, research about the gut microbiome has identified a potential culprit for the fibromyalgia experience and, surprisingly, it originates in the gut.
In a study on the microbiome in patients with fibromyalgia, they found that the diagnosis of fibromyalgia explained the difference in microbiome between people with and without fibromyalgia more than any demographic, dietary, medication, or medical history factor. In another study on mice, they found that when the mice were colonized with the gut microbes from people with fibromyalgia, they developed fibromyalgia-like symptoms. When they gave the mice a transplant of normal gut microbes the symptoms substantially improved.
What Changes Our Microbiomes?
The species of bacteria present in the gut change due to multiple factors including:
Hormone levels
Changes in diet
Food preservatives
Antibiotic usage
Stress
One source of stress I had not considered in the evolution of our microbiomes was how much the stress of physical disease impacts the microbiome and how much the microbiome influences the evolution of disease. When researchers induced a large stroke in mice, they found that it upset the balance of bacteria, decreasing the different types of bacterial species in the gut. This imbalance increased inflammation, which both increased the size of the injury (by about 60% in this study) in the brain and the amount of functional limitations the mouse had. In addition, when they transplanted healthy bacteria back into the gut, it improved outcomes for the mice who had strokes.
In this study, some animals also underwent a surgical procedure without inducing the stroke (called a sham surgery). These animals also had some, though less severe changes in the balance and diversity of bacteria. This calls attention to how important stress on the body is to the balance of bacteria in the gut. One other fascinating aspect of this study was they found that lymph cells from the intestines of the mice also migrated to the parts of the brain that were not getting enough oxygen due to the induced stroke. All of which is to say, the intestines and the brain are profoundly interconnected in ways we are just beginning to understand.
Fortunately, our gut microbiomes are usually able to adapt to many stresses and with support can often rebound from antibiotic treatment, stress, and processed foods. Next week, we’ll discuss more about how to support your microbiome through diet and lifestyle. I had planned to save that one for my paid subscribers, but I wanted to offer you a preview of what my new paid content will be like (and to be totally honest, I found it super interesting and wanted to shout it from the rooftops).
For the next month, I am running a special for paid subscriptions. A paid subscription is for you if:
You agree with me that true health is based on connection and relationship, but aren’t quite sure how to cultivate that in real life.
You want to learn from the experience of others with some simple (but maybe not easy) things to incorporate into your life to go from “meh” or “good enough” to THRIVING.
You love gut microbiomes and plants as much as me and want MORE. More paid subscribers=more time to dig into these fascinating topics.
Join as a paid subscriber by June 19 and earn 20% off forever. If finances are an issue, please reach out, we can discuss a further discount.




I was diagnosed with Crohn's disease 30 years ago and wish I had access to this information years ago. But it's never too late. I focus on my diet and gut biome and it has made a huge difference in my life.
Fascinating, thank you full pulling this together it’s clearly a lot of research and time. Look forward to the next one! K